Battle is breaking out in southwestern Ontario between three long-term care facilities and local public health, with health officials refusing to test elderly asymptomatic patients for COVID-19
Doctors at Ontario long-term care facilities face off with province over resident testing. This is a crucial issue.
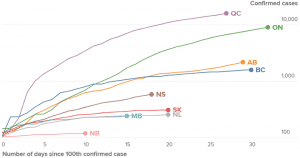
Source: April 17, 2020 Global News article entitled: “Canada is flattening the coronavirus curve. That’s ‘good news,’ expert explains.”
An April 7, 2020 Globe and Mail article is entitled: “Doctors for Ontario long-term care facilities face off with public health officials over resident testing.”
An excerpt reads:
A battle is breaking out in southwestern Ontario between three long-term care facilities and local public health, with health officials refusing to test elderly patients for COVID-19 if they don’t have any symptoms.
The doctor serving the facilities says on at least two occasions, Southwestern Public Health officials refused to pick up swabs from residents who were transferred into long-term care from hospitals.
The newly-admitted residents were asymptomatic for the coronavirus. The problem, says Dr. Barry Roth, is that elderly people can carry the deadly virus without showing or being able to express their symptoms, leading to fears of potential outbreaks among the most vulnerable population.
“We want to know what’s coming into our facility. … We don’t want to stick our head in the sand and say, ‘Ok let’s wait and see if they get symptoms,'” said Dr. Roth, medical director for Woodingford Lodge, which has three locations and a total of 228 residents.
“Our whole goal during this thing is let’s keep COVID-19 out of our facilities. These are our residents, we treat them like I would treat my parents.”
Mark Dager, the facilities’ director, said the Local Health Integration Network (LHIN), which helps co-ordinate patient care, asked the homes to take in elderly patients who were in hospitals, even for the short-term, to open up space for a potential influx of new coronavirus cases. He also said community admissions have not stopped amid the COVID-19 pandemic.
Ontario testing shortfall highlighted in April 8, 2020 CBC article
An April 8, 2020 CBC article is entitled: “Doug Ford blasts ‘unacceptable’ level of COVID-19 testing as Ontario cases top 5,000: Province sees largest single-day increase in cases since the outbreak began.”
An excerpt reads:
Ontario’s chief medical officer of health, Dr. David Williams, said there’s an expert group that will report very shortly on a strategy to expand the number of tests and further increase the capacity of testing centres.
Although Williams said the increased capacity will make long-term care workers and residents a priority, he added health officials also hope to expand testing within Indigenous populations, prisons and the province’s homeless population.
Williams also said the fewer tests seems to coincide with fewer people using the province’s telehealth service and its online assessment tool, which tells people whether they meet the criteria for COVID-19 testing.
“It may be evidence of some flattening,” he suggested, admitting he preferred to “be optimistic” in believing it could be due to fewer travellers and fewer people with symptoms.
“We’re not trying to limit (testing),” he insisted.
Williams cautioned that testing too widely would produce “biased” data that skew too heavily toward negative results when the goal is to reflect the population-at-large.
Critics alarmed by Ontario’s testing shortfall
An April 8, 2020 Canadian Press article carried by CityNews is entitled: “Critics alarmed by Ontario’s testing shortfall for COVID-19.”
An excerpt reads:
Ontario’s overly cautious approach to COVID-19 testing is endangering lives and hindering efforts to rein in soaring infections that are ravaging long-term care facilities, filling ICU beds and lurking silently in communities, say critics alarmed by the province’s admission that labs can handle nearly four times the number of tests they receive.
Dr. Camille Lemieux, chief of family medicine at the University Health Network, expressed frustration Wednesday over revelations the province has been sending roughly 3,500 tests a day to its labs of late, even though labs can accommodate 13,000 tests.
“You can’t make decisions in the dark, and you can’t make decisions based upon what you don’t know and I think any reasonable person would say that,” says Lemieux, who works out of downtown Toronto’s Western Hospital where she’s also the medical lead for the facility’s assessment centre.
U.S. nurses concerned about lack of testing
An April 8, 2020 Reuters article is entitled: “U.S. nurses who can’t get tested fear they are spreading COVID-19.”
An excerpt reads:
Until rapid testing is widely available, hospitals face a dilemma: Do they test staff with mild symptoms and keep them home for days as they await results? Or do they keep mildly ill – but desperately needed – staff at work to treat the rush of patients?
“It’s a different kind of triage,” said Caplan, the bioethics professor. “It’s precaution versus, ‘I need staff.’”
Rapid testing of all hospital employees could possibly decimate the workforce by revealing asymptomatic infected workers, several healthcare workers told Reuters. But it would also protect colleagues, patients and family members.
“It’s scary to come home and not know if you’re bringing it home to your family,” said Sydnie Boylan, a nurse at Hollywood Presbyterian Medical Center in Los Angeles.

Leave a Reply
Want to join the discussion?Feel free to contribute!