Intensive testing for COVID-19 is recommended by WHO; in Canada, public health messaging appears to emphasize restrictions on testing
Click here for previous posts about COVID-19 pandemic >
Introduction
I’ve been blogging about the coronavirus epidemic starting on March 7, 2020.
On March 17, 2020 I recorded the final segment of the CBC Radio “Here & Now” program from Toronto as well as that evening’s “The World at Six” broadcast. I listened to the recording using Adobe Premiere Pro and a set of earphones, made notes, and transcribed passages.
The experience of listening to such a recording on earphones provides a different experience as compared to hearing such a radio broadcast for the first time. Among the things I noticed was the use of layers of sound tracks to help move stories along.
These aspects of sound editing are evident the first time a person hears a broadcast, but when I listen to a recording, I can understand better how the layers of sound are put together. I note as well the similarities between news broadcasts on the one hand, and podcasts on the other.
I enjoy how each CBC broadcaster adopts a particular persona. The articulation, cadence, and rhythm entailed in news gathering and presentation is impressive.
I’ve also been reviewing some of the earlier posts at this website, concerned with the coronavirus pandemic.
I note that when we read something, even from a week ago, we realize how much is changing with each passing day. We realize how quickly the crisis is growing. We realize as well that once a particular narrative arc or trajectory is in place – for a given country, for example – then it follows that certain expectations may arise, regarding what kind of situation may be in place some weeks from now.
As I’ve been reading, I’ve found that particular news sources appeal to me more than others. Among many sources I like to follow are CBC, Reuters, ERR News in Estonia, and online medical journals such as the BMJ and Lancet.
WHO recommends focus above all on testing, isolation
A March 16, 2020 article at the WHO website is entitled: “WHO Director-General’s opening remarks at the media briefing on COVID-19 – 16 March 2020.”
An excerpt reads:
Social distancing measures can help to reduce transmission and enable health systems to cope.
Handwashing and coughing into your elbow can reduce the risk for yourself and others.
But on their own, they are not enough to extinguish this pandemic. It’s the combination that makes the difference.
As I keep saying, all countries must take a comprehensive approach.
But the most effective way to prevent infections and save lives is breaking the chains of transmission. And to do that, you must test and isolate.
You cannot fight a fire blindfolded. And we cannot stop this pandemic if we don’t know who is infected.
We have a simple message for all countries: test, test, test.
Test every suspected case.
Taiwan among handful of countries that have, to date, excelled in addressing coronavirus pandemic
A March 19, 2020 CBC article is entitled: “Is Taiwan’s impressive response to COVID-19 possible in Canada? As Canada struggles to flatten the curve, Taiwan has so far avoided a big curve.”
An excerpt reads:
The government has since barred all foreign travellers from entering the island.
Taiwan also created a health questionnaire that passengers accessed by scanning a QR code with their phones while still on planes as they were arriving.
Depending on their health status, they were sent a text message providing them with a health declaration pass to fast-track through immigration. Anyone at a higher risk of infection was urged to go into self-isolation at home and tracked via their cellphone to make sure they stayed there. False reporting of health information became a fineable offence.
“So this way they could triage a large number of passengers very quickly without lining up in the airport, which in itself is a risk,” Wang said.
After activating its central epidemic command centre on Jan. 20, the Taiwanese government integrated its health insurance database with its immigration database to create a real-time super data source that became central to identifying people most at risk of infection.
The database is accessible by health professionals and certain government officials in Taiwan and includes a patient’s travel history and personal information. Health officials regularly use text messaging to communicate with patients and follow up in person.
Interview with Toronto-area physician describing front-line experiences
A March 18, 2020 CBC article is entitled: “A Toronto doctor describes working on the front lines of the COVID-19 pandemic. Dr. Naheed Dosani says patients and health-care workers are exhibiting incredible kindness and patience.”
An excerpt reads:
Self-referral is appropriate to show up. We do have health-care worker referral as well. Currently, the criteria is for people who are experiencing symptoms of an upper-respiratory tract infection, or flu-like symptoms, and any of the following:
– Temperature greater than 38 C.
– Age over 60.
– Pregnant people.
– Health-care workers working on the front lines.
– And folks who have been in touch with someone who is [a] probable or confirmed diagnosis.
We saw 198 individuals on that shift, and 124 received testing. When people didn’t receive testing, I have to say, people were grateful. They were respectful. They were understanding that there may not be enough test kits for everyone at this time and that we have to heed public health advice on who gets the testing.
I heard an interview with Dr. Naheed Dosani in the CBC Radio segment that I recorded on March 17, 2020. In the interview, the front-line physician is asked about restrictions in testing for COVID-19 in the setting in which he was working. His reply was that he’s not an epidemiologist and that we need to put our trust in public health agencies and infectious disease experts. He said we need to put our faith in things like testing criteria at coronavirus assessment centres and the need for social distancing.
An additional excerpt from the above-noted March 18, 2018 CBC article is of interest with regard to testing; I note that the CBC reporter made a point of seeking to explore this topic at some depth:
Question from interviewer: You said that there was not enough test kits at this point. And that’s a great concern, isn’t it? Because we heard from [Tedros Adhanom], the head of the World Health Organization, this week. He said: “You cannot fight a fire blindfolded. And we cannot stop this pandemic if we don’t know who is infected. We have a simple message for all countries: test, test, test.” And we’re seeing that in South Korea, where there’s 270,000 people who have been tested. Other places where it’s less. In Canada, we have … just shy of 900 tests … per million of people [according to the National Post]. That’s high, but not as high as perhaps other countries are doing. Do you think that that’s a problem?
Answer: I should note while I’m not a public health specialist or infectious disease specialist, my experience working on the front lines at our assessment centre at William Osler Health System was that we definitely had enough tests for the individuals who were meeting criteria as set out by our public health experts.
My initial impression is that deference to authority with reference to testing restrictions is not fully warranted. Not all public health experts would agree that current restrictions on testing makes sense. I do agree there is tremendous value in compassion, mutual respect, and in working closely together.
Role of mild or asymptomatic infections prior to widespread travel restrictions in China
A March 16, 2020 MedPage Today article is entitled: “Over 85% of COVID-19 Infections in China Went Undetected Early On. Number of mild or asymptomatic infections emphasizes need for mitigation measures.”
An excerpt reads:
Prior to widespread travel restrictions in China, more than 85% of COVID-19 coronavirus infections went unnoticed, a modeling study suggested.
Only 14% of COVID-19 infections were documented in the two weeks prior to implementation of these widespread travel restrictions, meaning that the majority were people with mild symptoms or who were asymptomatic and who never sought care, reported Jeffrey Shaman, PhD, of Columbia University in New York City, and colleagues.
COVID-19 in the context of climate change
A March 17, 2020 London Review of Books article is entitled: “After Covid-19, the Climate.”
An excerpt reads:
By late last year, it seemed clear that decades of attempts to coax governments and business leaders into taking seriously the risks posed by the climate crisis were leading nowhere. Yet faced with the far more immediate threats posed by a global pandemic, states that for decades had been committed to neoliberal thinking have slowly begun to embrace such radically old-fashioned ideas as planning for the future, relying on scientific expertise, or calling on their constituents to make sacrifices in order to protect vulnerable members of society. Environmental campaigners and journalists have begun to document the effects that the shut-down of factories, cancellation of large conferences, postponement of sporting events, and limitations on freedom of movement have had on carbon emissions.
Relationship between COVID-19 and world history of land use practices
A March 18, 2020 Globe and Mail article is entitled: “To understand COVID-19 transmission, we have to understand our wastewater.”
An excerpt reads:
Since then, good science and engineering have helped us build integrated systems that link drinking, waste and storm water management. In ideal circumstances, these systems remove disease-causing contaminants from drinking water sources. Our urban wastewater treatment systems then clean our waste tap and toilet water (water that’s often combined with storm water runoff from rain or melting snow) to make it safe enough to release back in to surrounding streams, rivers, lakes and oceans. Drinking water and wastewater treatment is one of our great public-health success stories.
Despite this success, water supply systems around the world face two persistent and interconnected problems that have major health implications. Growing urban populations are combining with climate change to put ever greater demands on wastewater services; and we’re fighting a continuing battle to stay ahead of the constantly evolving pathogens that can make us sick.
Wastewater treatment plants may be built too small for growing populations or not maintained because of high costs. Also, climate change is causing more intense, frequent rainstorms. Particularly in concrete-covered cities, storm water can easily infiltrate and overload a sanitary system, causing the release of untreated wastewater into surrounding waters.
For example, the low-lying city of Wuhan, China – where the COVID-19 pandemic originated – paved over almost 100 naturally occurring lakes in a rush toward massive urbanization. Wuhan also has an abysmal wastewater treatment system.
Surge capacity may be limited
A March 19, 2020 New York Times article is entitled: “A New York Doctor’s Coronavirus Warning: The Sky Is Falling. Alarmist is not a word anyone has ever used to describe me before. But this is different.”
An excerpt reads:
On the front lines, patients are lining up outside of our emergency rooms and clinics looking to us for answers — but we have few. Only on Friday did coronavirus testing become more readily available in New York, and the tests are still extremely limited. Right next to my office in the hospital, a lab is being repurposed with hopes of a capability to run 1,000 tests a day. But today, and likely tomorrow, even M.D.s do not have straightforward access to testing across the country. Furthermore, the guidelines and criteria for testing are changing almost daily. Our health care system is mired in situational uncertainty. The leadership of our hospital is working tirelessly — but doctors on the ground are pessimistic about our surge capacity.
Comparisons among curve-flattening efforts
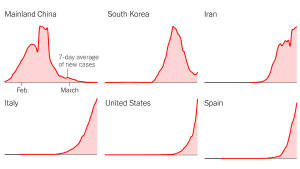
The image is from a March 19, 2020 New York Times article entitled: “Which Country Has Flattened the Curve for the Coronavirus?” I came across the image at a tweet by Jennifer Mercieca @jenmercieca who wrote: “I was looking for a comparative chart like this yesterday, and here it is today: Which Country Has Flattened the Curve for the Coronavirus?”
A March 19, 2020 New York Times article is entitled: “Which Country Has Flattened the Curve for the Coronavirus?”
An excerpt reads:
Despite their close proximity to China, Singapore, Hong Kong and Taiwan have managed to keep the number of cases down with some success, through vigilant monitoring and early intervention.
But recent spikes in those places suggest that they are still at risk. For example, 21 of the 23 new cases in Taiwan and at least 13 of the new cases in Hong Kong on Wednesday were people who had recently traveled overseas.
More countries are now implementing travel bans or mandatory quarantine for returning travelers, as the pandemic continues to ravage the world, sickening more than 210,000 people as of Wednesday evening.
In the United States and five other countries, the number of known coronavirus cases is still growing rapidly. They have all reported more than 4,000 new cases in the past week.
Distributive justice in treatment of novel coronavirus
A March 16, 2020 New York Review of Books article is entitled: “What ‘Distributive Justice’ Means for Doctors Treating Covid-19.”
An excerpt reads:
What doctors call the “natural history” of Covid-19 can be envisioned as four stages; most people’s individual cases will stop at the first or, at most, the second stage, while an unlucky minority will experience the third, or all four. First, there is either an asymptomatic or a mildly symptomatic, nonspecifically “flu-like” illness. In Guangzhou province in China, researchers found that the median incubation period is about four days before symptoms, if any, set in. A portion of those with symptomatic, positive disease then experience a second stage: viral pneumonia, often visible on chest X-rays and CT scans by the varying degrees of inflammation of the lung’s interstitium, the connecting and supportive tissues that line the small airways and blood vessels where oxygen and carbon dioxide are exchanged between blood and air with each breath and heartbeat.
The third stage is a process called acute respiratory distress syndrome (ARDS), a rapid and overwhelming inflammatory response that the body mounts against a perceived foreign invader. ARDS is rare but not specific to Covid-19, and can happen in cases as disparate as near-drownings, blunt trauma, overdoses, and infections of any kind, including sometimes the most innocuous-seeming pathogens. (I once saw a patient die of ARDS after catching a fairly standard case of “mono” in college.) Based on data from China and Italy, about 15–20 percent of Covid-19-positive patients who are sick enough to need the hospital will need intensive care unit-level care for severe interstitial pneumonia or full-blown ARDS.
The fourth, rarest, and most frightening stage of Covid-19 is rapid heart failure and cardiac arrest, often after the pneumonia or ARDS has nearly resolved. While we need more organized research to avoid cognitive biases (which can occur by our fixating on particularly memorable but atypical cases), early reports from front-line providers in disease hotspots suggest that these last cases happen to two broad categories of people: relatively healthy adults of about thirty to fifty years of age, and older patients with cardiovascular disease.
Hospital labs stepping in to help build testing capacity
A March 21, 2020 Globe and Mail article is entitled: “Hospital-based labs mobilize to test for COVID-19 and alleviate backlog.”
An excerpt reads:
Most people who contract COVID-19 will experience relatively minor symptoms and may not realize they’re infected, which means they are likely to go out in public and spread the disease to others, said Janine McCready, an infectious diseases physician at Toronto’s Michael Garron Hospital. That’s why so many experts are so insistent on the need for increased testing capacity in Canada: in order to understand the scope of the problem and stop transmission, officials need a realistic picture of how many people are infected, Dr. McCready said.
“Before you even realize you have it, you could have already exposed a number of other people,” she said.
Dr. McCready said she has contacted numerous patients in recent days who were surprised to learn they tested positive for COVID-19, as their symptoms were so mild.
She and other infectious disease experts say there is widespread community transmission of the virus in Ontario, meaning infections with no known link to international travel. Despite this, Ontario officials have stopped short of confirming community spread in the province.

Leave a Reply
Want to join the discussion?Feel free to contribute!