South Korea and Germany are doing extensive COVID-19 testing; Province of Ontario has not been doing much testing at all
We can learn much of interest about how different countries approach planning and governance, if we consider how each has responded to the COVID-19 pandemic.
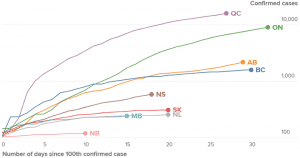
Source: April 17, 2020 Global News article entitled: “Canada is flattening the coronavirus curve. That’s ‘good news,’ expert explains.”
Many published accounts are available.
Among them is a March 29, 2020 Guardian article entitled: “The missing six weeks: how Trump failed the biggest test of his life.”
An excerpt reads:
A week after that, the Wall Street Journal published an opinion article by two former top health policy officials within the Trump administration under the headline Act Now to Prevent an American Epidemic. Luciana Borio and Scott Gottlieb laid out a menu of what had to be done instantly to avert a massive health disaster.
Top of their to-do list: work with private industry to develop an “easy-to-use, rapid diagnostic test” – in other words, just what South Korea was doing.
It was not until 29 February, more than a month after the Journal article and almost six weeks after the first case of coronavirus was confirmed in the country that the Trump administration put that advice into practice. Laboratories and hospitals would finally be allowed to conduct their own Covid-19 tests to speed up the process.
Those missing four to six weeks are likely to go down in the definitive history as a cautionary tale of the potentially devastating consequences of failed political leadership. Today, 86,012 cases have been confirmed across the US, pushing the nation to the top of the world’s coronavirus league table – above even China.
Lag in ordering of supplies in U.S.
An April 6, 2020 Associated Press article is entitled: “Lost Time: How coronavirus spread while supply orders lagged.”
An excerpt reads:
The government’s stockpile of critically needed medical supplies and equipment is nearly drained just as the numbers of people infected with the coronavirus and in need of critical care is surging. Back in January, the first alarms were sounding about the outbreak in China. In time, it would become a global pandemic. An Associated Press review has found that the Trump administration squandered precious months before bolstering the federal stockpile of urgently needed medical supplies and equipment.
Germany like South Korean doing well with new coronavirus testing
Some features of Germany’s approach to COVID-19 appear to be unique, according to published reports.
An April 4, 2020 New York Times article is entitled: “A German Exception? Why the Country’s Coronavirus Death Rate Is Low.”
The subhead reads: “The pandemic has hit Germany hard, with more than 92,000 people infected. But the percentage of fatal cases has been remarkably low compared to those in many neighboring countries.”
An excerpt reads:
By now, Germany is conducting around 350,000 coronavirus tests a week, far more than any other European country. Early and widespread testing has allowed the authorities to slow the spread of the pandemic by isolating known cases while they are infectious. It has also enabled lifesaving treatment to be administered in a more timely way.
“When I have an early diagnosis and can treat patients early — for example put them on a ventilator before they deteriorate — the chance of survival is much higher,” Professor Kräusslich said.
Medical staff, at particular risk of contracting and spreading the virus, are regularly tested. To streamline the procedure, some hospitals have started doing block tests, using the swabs of 10 employees, and following up with individual tests only if there is a positive result.
At the end of April, health authorities also plan to roll out a large-scale antibody study, testing random samples of 100,000 people across Germany every week to gauge where immunity is building up.
One key to ensuring broad-based testing is that patients pay nothing for it, said Professor Streeck. This, he said, was one notable difference with the United States in the first several weeks of the outbreak. The coronavirus relief bill passed by Congress last month does provide for free testing.
April 9, 2020 Reuters article highlights Germany’s approach to virus defences
An April 9, 2020 Reuters article is entitled: “Pass the salt: The minute details that helped Germany build virus defences.”
An excerpt reads:
The time Germany bought may have saved lives, scientists say. Its first outbreak of locally transmitted COVID-19 began earlier than Italy’s, but Germany has had many fewer deaths. Italy’s first detected local transmission was on Feb. 21. By then Germany had kicked off a health ministry information campaign and a government strategy to tackle the virus which would hinge on widespread testing. In Germany so far, more than 2,100 people have died of COVID-19. In Italy, with a smaller population, the total exceeds 17,600.
Ontario slow to start with testing
Of related interest is an April 3, 2020 Reuters article entitled “Ontario lab design left province short of coronavirus testing supplies.”
An excerpt reads:
TORONTO (Reuters) – Ontario, Canada’s most heavily populated region, has been lagging other Canadian provinces in testing for the coronavirus because in the early weeks of the outbreak its public labs relied heavily on a single company for needed chemicals.
The province is ramping testing back up, focused on finding patients who could have had the largest impact on others, such as healthcare workers. But the slowdown led to thousands of backlogged tests.
“There are real restrictions on who is being tested, so test results are not a real accurate measure of how widespread the infection is,” said Jane Philpott, a former federal health minister and doctor who is doing clinical work.
“There’s an unknown number of people who have had respiratory symptoms and probably had COVID infections that have not been tested.”
As of Wednesday, Ontario had tested 4,188 per million residents, less than every Canadian province except New Brunswick and Prince Edward Island, which have far fewer cases. Alberta had tested 11,139 per million, and Quebec 8,216 per million.
An April 8, 2020 CBC article reads: “Ontario conducting fewer COVID-19 tests daily as cases keep climbing: Public health experts urge province to test more widely, while health minister promises increase ‘soon.'”
An excerpt reads reads:
But Ontario has not tested anywhere near that many people in a single day yet, and there are no signs of when it will ramp up testing to use the full lab capacity.
One sign of how narrowly Ontario’s testing is focused on the most likely cases: nearly 15 per cent of the test results announced on Tuesday were positive. Quebec’s confirmed cases are running at about nine per cent of all tests, and in B.C. it’s less than three per cent.
Testing gaps in U.S.
An April 6, 2020 New York Times article is entitled: “Delays and Shortages Exacerbate Coronavirus Testing Gaps in the U.S.: The lack of coronavirus test supplies, and long waits for results, has caused serious problems for many hospitals, even as new and faster tests come onto the market.”
An excerpt reads:
“Many local communities are flying blind, making decisions in the absence of full information largely due to the failure of the federal government to provide sufficient testing capacity,” said Chrissie Juliano, executive director of the Big Cities Health Coalition, which represents executives in 30 urban public health departments, among them Boston, Chicago, Los Angeles, New York City and Seattle. “This testing shortage, and lack of available information about the actual burden of the virus, has set our country’s response back by an order of magnitude we will never know.”
Previous experience with HIV and tuberculosis prepares South Africa for COVID-19 testing
An April 6, 2020 Associated Press article is entitled: “South Africa’s TB, HIV history prepares it for virus testing.”
An excerpt reads:
JOHANNESBURG (AP) — South Africa, one of the world’s most unequal countries with a large population vulnerable to the new coronavirus, may have an advantage in the outbreak, honed during years battling HIV and tuberculosis: the know-how and infrastructure to conduct mass testing.
Health experts stress that the best way to slow the spread of the virus is through extensive testing, the quick quarantine of people who are positive, and tracking who those people came into contact with.
“We have a simple message for all countries: test, test, test,” Tedros Adhanom Ghebreyesus, director-general of the World Health Organization and a former Ethiopian health minister, said recently.
South Africa has begun doing just that with mobile testing units and screening centers established in the country’s most densely populated township areas, where an estimated 25% of the country’s 57 million people live.
Outcomes in California compared to New York
An April 6, 2020 Globe and Mail article is entitled: “Why isn’t California’s coronavirus crisis as bad as New York’s? Size doesn’t tell the whole story. Density, decisive action and luck are all factors in why the West Coast’s outbreaks are less terrifying than the East’s so far.”
An excerpt reads:
Yet New York Governor Andrew Cuomo’s order closing most non-essential businesses came almost a week after the Bay Area’s shelter-in-place order. That delay is “an eternity for an epidemic that is growing exponentially,” Prof. Bettencourt said.
In California, there are signs that the early efforts at social distancing are working. “Look outside. It looks like Christmas Day,” said University of California, San Francisco epidemiologist George Rutherford. “There are no leaf blowers. The gardeners have gone. Nobody’s pounding nails into their roofs. People are at home and they really are sheltered in place.”
Hospitals in San Francisco have yet to be overwhelmed with patients. While the state has dramatically expanded testing in recent weeks, the percentage of tests coming back positive has remained stable at about 6 per cent.
The outcomes from the two states are expected to be dramatic, with the University of Washington’s Institute for Health Metrics and Evaluation projecting California will likely see about 5,000 deaths from COVID-19 this year, compared with more than 16,000 in New York.
Larger topic of public health leadership
A subsequent post, which addresses public health leadership cultures, is entitled:
Sobering thoughts, regarding distinctions in public health leadership culture
Of related interest, an April 20, 2020 Atlantic article is entitled: “The Secret to Germany’s COVID-19 Success: Angela Merkel Is a Scientist; The chancellor’s rigor in collating information, her honesty in stating what is not yet known, and her composure are paying off.’
An excerpt reads:
The virus is still far from defeated, and no one knows what challenges lie ahead for Germany, or the rest of the world. But judging by Merkel’s approach – her rigor in collating information, her honesty in stating what is not yet known, and her composure – she may someday be remembered not as Germany’s greatest scientist, but as its scientist in chief: the political leader who executed, celebrated, and personified evidence-based thinking when it mattered most.

Leave a Reply
Want to join the discussion?Feel free to contribute!