COVID-19 testing is an absolute priority – including of asymptomatic individuals; not much testing is happening in Ontario right now
*
Updates: An April 9, 2020 Globe and Mail article is entitled: “Ontario now recommends COVID-19 tests for anyone moving into long-term care facility.”
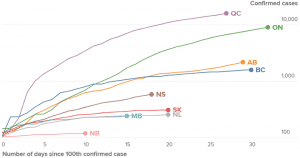
Source: April 17, 2020 Global News article entitled: “Canada is flattening the coronavirus curve. That’s ‘good news,’ expert explains.”
An April 10, 2020 CBC article is entitled: “Ontario plans for 16,000 COVID-19 tests daily by May 6 amid mounting criticism over low testing: Provincial officials say they will be targeting vulnerable populations.”
An excerpt reads:
The expanded guidance stopped short of a call by Ford earlier in the week for every long-term care resident, front-line health-care worker and first responder to be tested.
Friday’s strategy also reiterated the province’s stance that asymptomatic people who are not at high-risk should not be tested as it could provide a false negative, and it would waste valuable resources.
An April 17, 2020 Globe and Mail article is entitled: “Toronto Public Health struggling to keep up with contact tracing, doctors say.”
An excerpt reads:
Public health staff in Canada’s largest city are struggling to keep up with the vital work known as contact tracing, or alerting those associated with people who test positive for COVID-19 in a bid to curb its spread, some Toronto doctors say.
Doctors say that individuals who test positive can wait for days without a follow-up call from Toronto Public Health’s contact tracers, who perform the detective-like task of tracking a patient’s steps. In some cases, this means that friends or co-workers of a positive case are not being promptly instructed to self-isolate for the mandated 14 days.
[End of updates]
*
At the current post I will share links from previous posts about COVID-19 and will add a few updates.
How we use language determines the effectiveness of COVID-19 messages; a related topic concerns dealing with misinformation
March 26, 2020: As Suzanne Wertheim, linguistic anthropologist, notes: Our linguistic choices can amplify a message. Or they can muddy it, and lessen its impact
A related topic concerns how best to counter COVID-19 rumours and misinformation
A March 10, 2020 Undark article is entitled: “Opinion: Don’t Just Debunk Covid-19 Myths. Learn From Them: The tactic of simply throwing facts at the misinformation problem can be ineffective, and even counterproductive.”
Instead of viewing rumors and myths as misperceptions that can be suppressed with accurate information, we should treat them as opportunities to understand — and respond to — the legitimate anxieties of the people who adopt and share them. In other words, we should look at them as valuable feedback that can help improve our own reporting and messaging.
An April 7, 2020 STAT News article is entitled: “Misinformation about an outbreak like Covid-19 is important public health data.”
The spread of information — and misinformation — has been playing a crucial role throughout the unfolding coronavirus outbreak and should serve as a wake-up call for scientists who model epidemics. With every outbreak of a new pathogen comes a race to estimate its transmissibility, which scientists, the media, and the public use to compare the new threat to known enemies.
What this approach fails to capture is the extent to which disease epidemics are shaped by unique interactions between biological and social factors — and that social communication and behaviors during an outbreak are just as important to public health as tests and diagnoses.
Recommended COVID-19 strategy is to respond early and aggressively
Below are links to posts dealing with topics related to COVID-19. At the end of the current posts are links to recent articles about testing for the coronavirus.
March 7, 2020: This American Life Episode 695: Everyone’s a Critic – Act Two – “Mr. Chen Goes to Wuhan
March 13, 2020: It’s best to respond early and aggressively to COVID-19
March 15, 2020: The result, notes Dr. David Fisman, U of T professor of epidemiology in reference to CDC, is basically a decapitated public health system
March 24, 2020: Rate of known coronavirus cases in Taiwan is one-fifth the rate of known cases in the United States
March 28, 2020: CBC Second Opinion newsletter presents exemplary coronavirus (and related health news) updates
April 4, 2020: Sweden’s approach to COVID-19 has been changing
April 5, 2020: Evidence-based practice requires a robust methodological framework; otherwise, we are dealing with empty, potentially lethal rhetoric
April 7, 2020: Sobering thoughts, regarding distinctions in public health leadership culture
Testing matters hugely; some jurisdictions are performing well in this area, some are not
March 20, 2020: March 20, 2020 New York Times article provides comprehensive overview of Covid-19 testing narrative as it unfolds
March 20, 2020: Countries that do well in current crisis have good testing and a good system for tracking down of people who may have been infected
March 21, 2020: CBC Second Opinion article notes mass COVID-19 testing is key to stopping spread
April 4, 2020: Taiwan has got it right
April 5, 2020: South Korea and Germany are doing extensive COVID-19 testing; Province of Ontario has not been doing much testing at all
Doctors at Ontario long-term care facilities face off with province over resident testing
An April 7, 2020 Globe and Mail article is entitled: “Doctors for Ontario long-term care facilities face off with public health officials over resident testing.”
An excerpt reads:
A battle is breaking out in southwestern Ontario between three long-term care facilities and local public health, with health officials refusing to test elderly patients for COVID-19 if they don’t have any symptoms.
The doctor serving the facilities says on at least two occasions, Southwestern Public Health officials refused to pick up swabs from residents who were transferred into long-term care from hospitals.
The newly-admitted residents were asymptomatic for the coronavirus. The problem, says Dr. Barry Roth, is that elderly people can carry the deadly virus without showing or being able to express their symptoms, leading to fears of potential outbreaks among the most vulnerable population.
“We want to know what’s coming into our facility. … We don’t want to stick our head in the sand and say, ‘Ok let’s wait and see if they get symptoms,'” said Dr. Roth, medical director for Woodingford Lodge, which has three locations and a total of 228 residents.
“Our whole goal during this thing is let’s keep COVID-19 out of our facilities. These are our residents, we treat them like I would treat my parents.”
Mark Dager, the facilities’ director, said the Local Health Integration Network (LHIN), which helps co-ordinate patient care, asked the homes to take in elderly patients who were in hospitals, even for the short-term, to open up space for a potential influx of new coronavirus cases. He also said community admissions have not stopped amid the COVID-19 pandemic.
“Our staff are coming to work each and every day and they are presented with so much uncertainty,” Mr. Dager said. “We need to do our due diligence and even swab the asymptomatic individuals.”
Ontario testing shortfall highlighted in April 8, 2020 CBC article
An April 8, 2020 CBC article is entitled: “Doug Ford blasts ‘unacceptable’ level of COVID-19 testing as Ontario cases top 5,000: Province sees largest single-day increase in cases since the outbreak began.”
An excerpt reads:
Ontario’s chief medical officer of health, Dr. David Williams, said there’s an expert group that will report very shortly on a strategy to expand the number of tests and further increase the capacity of testing centres.
Although Williams said the increased capacity will make long-term care workers and residents a priority, he added health officials also hope to expand testing within Indigenous populations, prisons and the province’s homeless population.
Williams also said the fewer tests seems to coincide with fewer people using the province’s telehealth service and its online assessment tool, which tells people whether they meet the criteria for COVID-19 testing.
“It may be evidence of some flattening,” he suggested, admitting he preferred to “be optimistic” in believing it could be due to fewer travellers and fewer people with symptoms.
“We’re not trying to limit (testing),” he insisted.
Williams cautioned that testing too widely would produce “biased” data that skew too heavily toward negative results when the goal is to reflect the population-at-large.
Critics alarmed by Ontario’s testing shortfall
An April 8, 2020 Canadian Press article carried by CityNews is entitled: “Critics alarmed by Ontario’s testing shortfall for COVID-19.”
An excerpt reads:
Ontario’s overly cautious approach to COVID-19 testing is endangering lives and hindering efforts to rein in soaring infections that are ravaging long-term care facilities, filling ICU beds and lurking silently in communities, say critics alarmed by the province’s admission that labs can handle nearly four times the number of tests they receive.
Dr. Camille Lemieux, chief of family medicine at the University Health Network, expressed frustration Wednesday over revelations the province has been sending roughly 3,500 tests a day to its labs of late, even though labs can accommodate 13,000 tests.
“You can’t make decisions in the dark, and you can’t make decisions based upon what you don’t know and I think any reasonable person would say that,” says Lemieux, who works out of downtown Toronto’s Western Hospital where she’s also the medical lead for the facility’s assessment centre.
U.S. nurses concerned about lack of testing
An April 8, 2020 Reuters article is entitled: “U.S. nurses who can’t get tested fear they are spreading COVID-19.”
An excerpt reads:
Until rapid testing is widely available, hospitals face a dilemma: Do they test staff with mild symptoms and keep them home for days as they await results? Or do they keep mildly ill – but desperately needed – staff at work to treat the rush of patients?
“It’s a different kind of triage,” said Caplan, the bioethics professor. “It’s precaution versus, ‘I need staff.’”
Rapid testing of all hospital employees could possibly decimate the workforce by revealing asymptomatic infected workers, several healthcare workers told Reuters. But it would also protect colleagues, patients and family members.
“It’s scary to come home and not know if you’re bringing it home to your family,” said Sydnie Boylan, a nurse at Hollywood Presbyterian Medical Center in Los Angeles.
April 9, 2020 Stat News article refers to U.S. hit-or-miss response
An April 9, 2020 Stat News article is entitled: “‘We’re being put at risk unnecessarily’: Doctors fume at government response to coronavirus pandemic.”
An excerpt reads:
STAT interviewed more than a dozen physicians and scientists around the country, and one after another, they leveled strikingly similar critiques at both the federal and local levels: That the Trump administration neglected scientists and public health experts and downplayed the severity of the disease, helping stoke a spread of misinformation. That many state leaders, toeing party lines, were too paralyzed to act in a timely fashion. And that the Centers for Disease Control and Prevention, once a venerable institution, bungled a critical component of pandemic control — diagnostic testing.

Leave a Reply
Want to join the discussion?Feel free to contribute!